Aase syndrome or Aase-Smith syndrome is a rare inherited disorder characterized by anemia with some joint and skeletal deformities. The anemia is caused by underdevelopment of the bone marrow, which is where blood cells are formed.
It is named after the American pediatricians Jon Morton Aase and David Weyhe Smith.
Some of the symptoms it manifests are mildly slowed growth, pale skin, delayed closure of fontanelles (soft spots), narrow shoulders, triple jointed thumbs, absent or small knuckles, decreased skin creases at finger joints, inability to fully extend the joints from birth (congenital contractures), cleft palate, deformed ears, droopy eye lids.
[External Links]
Information complete with diagnosis and more from wrongdiagnosis.com
Information from umm.edu
Related Websites
Colic
Colic or Abdominal cramps are caused by involuntary muscle contractions that can be very painful. Cramps or pain may occur when any of the muscles in the abdomen or in the walls of the bowels are stretched or strained. Because many internal organs are located in this region, it is hard to know the exact cause of cramping without further investigation.
Cramps in the abdomen can occur from: food moving through the stomach and intestines, mild food poisoning that is usually accompanied by diarrhea, stress and anxiety, gastritis (an inflammation of the stomach lining), menstruation, disease or infection in the uterus, and pregnancy, childbirth, and changing hormone levels during breast-feeding.
Symptoms such as rumbling and gurgling noises, belching, passing gas, nausea, or vomiting may be felt. Diarrhea or constipation may occur. Urinary problems or loss of hunger may also be present.
More serious conditions, such as appendicitis or gall bladder attacks, will usually cause severe and constant cramping. Cramping that last more than one-half hour, and are not related to menstruation or a known digestive condition (such as colitis), requires medical attention.
[External Links]
Information from uihealthcare.com
Information from wrongdiagnosis.com
Information from MedlinePlus
Cramps in the abdomen can occur from: food moving through the stomach and intestines, mild food poisoning that is usually accompanied by diarrhea, stress and anxiety, gastritis (an inflammation of the stomach lining), menstruation, disease or infection in the uterus, and pregnancy, childbirth, and changing hormone levels during breast-feeding.
Symptoms such as rumbling and gurgling noises, belching, passing gas, nausea, or vomiting may be felt. Diarrhea or constipation may occur. Urinary problems or loss of hunger may also be present.
More serious conditions, such as appendicitis or gall bladder attacks, will usually cause severe and constant cramping. Cramping that last more than one-half hour, and are not related to menstruation or a known digestive condition (such as colitis), requires medical attention.
[External Links]
Information from uihealthcare.com
Information from wrongdiagnosis.com
Information from MedlinePlus
11 Beta Hydroxylase Deficiency
A steroid hydroxylase system found in adrenal tissues. It catalyzes the 11-hydroxylation of steroids in the presence of molecular oxygen and consists of an NADPH-specific flavoprotein, a non-heme iron protein, and cytochrome P-450. Its deficiency is a cause of congenital adrenal hyperplasia.
[External Links]
Information from gpnotebook.co.uk
Information from OMIM
[External Links]
Information from gpnotebook.co.uk
Information from OMIM
Aneurysm
 An aneurysm (or aneurism) is a localized, blood-filled dilation (balloon-like bulge) of a blood vessel caused by disease or weakening of the vessel wall.
An aneurysm (or aneurism) is a localized, blood-filled dilation (balloon-like bulge) of a blood vessel caused by disease or weakening of the vessel wall.Aneurysms most commonly occur in arteries at the base of the brain (the circle of Willis) and in the aorta (the main artery coming out of the heart, a so-called aortic aneurysm). As the size of an aneurysm increases, there is an increased risk of rupture, which can result in severe hemorrhage or other complications including sudden death.
Diagnosis of a ruptured cerebral aneurysm is commonly made by finding signs of subarachnoid hemorrhage on a CT scan (Computed Tomography, sometimes called a CAT scan, a computerized test that rapidly X-rays the body in cross-sections, or slices, as the body is moved through a large, circular machine). If the CT scan is negative but a ruptured aneurysm is still suspected, a lumbar puncture is performed to detect blood in the cerebrospinal fluid (CSF). Computed Tomography Angiography (CTA) is an alternative to the traditional method and can be performed without the need for arterial catheterization. This test combines a regular CT scan with a contrast dye injected into a vein. Once the dye is injected into a vein, it travels to the brain arteries, and images are created using a CT scan. These images show exactly how blood flows into the brain arteries.
[External Links]
Information from nhlbi.nih.gov
Information from MedlinePlus
Information from mercksource.com
Suggestions/Requests/Comments
Please leave us your suggestions, requests, or comments. Please do not use this column to ask for medical advice, and please don't ask for things beyond our scope. We will try to respond to every suggestions, and requests you write here, but we cannot guarantee that all requests will be granted.
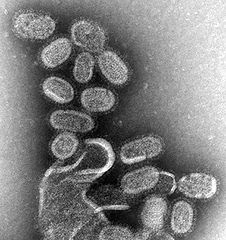
Spanish Flu
 The 1918 flu pandemic (commonly referred to as the Spanish flu) was an influenza pandemic that spread to nearly every part of the world. It was caused by an unusually severe and deadly Influenza A virus strain of subtype H1N1. Historical and epidemiologic data are inadequate to identify the geographic origin of the virus. Most of its victims were healthy young adults, in contrast to most influenza outbreaks which predominantly affect juvenile, elderly, or otherwise weakened patients. The pandemic lasted from March 1918 to June 1920, spreading even to the Arctic and remote Pacific islands. It is estimated that anywhere from 20 to 100 million people were killed worldwide, or the approximate equivalent of one third of the population of Europe, more than double the number killed in World War I. This extraordinary toll resulted from the extremely high illness rate of up to 50% and the extreme severity of the symptoms, suspected to be caused by cytokine storms.
The 1918 flu pandemic (commonly referred to as the Spanish flu) was an influenza pandemic that spread to nearly every part of the world. It was caused by an unusually severe and deadly Influenza A virus strain of subtype H1N1. Historical and epidemiologic data are inadequate to identify the geographic origin of the virus. Most of its victims were healthy young adults, in contrast to most influenza outbreaks which predominantly affect juvenile, elderly, or otherwise weakened patients. The pandemic lasted from March 1918 to June 1920, spreading even to the Arctic and remote Pacific islands. It is estimated that anywhere from 20 to 100 million people were killed worldwide, or the approximate equivalent of one third of the population of Europe, more than double the number killed in World War I. This extraordinary toll resulted from the extremely high illness rate of up to 50% and the extreme severity of the symptoms, suspected to be caused by cytokine storms.The disease was first observed at Fort Riley, Kansas, United States, on March 4, 1918, and Queens, New York, on March 11, 1918. In August 1918, a more virulent strain appeared simultaneously in Brest, France, in Freetown, Sierra Leone, and in the U.S. at Boston, Massachusetts. The Allies of World War I came to call it the Spanish flu, primarily because the pandemic received greater press attention after it moved from France to Spain in November 1918. Spain was not involved in the war and had not imposed wartime censorship.
Scientists have used tissue samples from frozen victims to reproduce the virus for study. Given the strain's extreme virulence there has been controversy regarding the wisdom of such research. Among the conclusions of this research is that the virus kills via a cytokine storm, which explains its unusually severe nature and the unusual age profile of its victims (the virus caused an overreaction of the body's immune system—the strong immune systems of young adults ravaged the body, while the weaker immune systems of children and middle-aged adults caused fewer deaths).
[External Links]
Information from virus.stanford.edu
Link to March 21, 1997 news regarding Spanish Flu
Scrofula

Scrofula is any of a variety of skin diseases; in particular, a form of tuberculosis, affecting the lymph nodes of the neck. It is often informally or historically known as 'King's Evil', referring to the method of treatment many sufferers used, in some cases in England up to the reign of King Charles II. In adults it is caused by Mycobacterium tuberculosis and in children by nontuberculous mycobacteria. The word comes from the Latin scrofula, meaning brood sow.
Scrofula is the term used for tuberculosis of the neck, or, more precisely, a cervical tuberculous lymphadenopathy. Scrofula is usually a result of an infection in the lymph nodes, known as lymphadenitis and is most often observed in immunocompromised patients (about 50% of cervical tuberculous lymphadenopathy). About 95% of the scrofula cases in adults are caused by Mycobacterium tuberculosis, but only 8% of cases in children. The rest are caused by atypical mycobacterium (Mycobacterium scrofulaceum) or nontuberculous mycobacterium (NTM).
The most usual signs and symptoms are the appearance of a chronic, painless mass in the neck, which is persistent and usually grows with time. The mass is referred to as a "cold abscess", because there is no accompanying local color or warmth and the overlying skin acquires a violaceous (bluish-purple) color. NTM infections do not show other notable constitutional symptoms, but scrofula caused by tuberculosis is usually accompanied by other symptoms of the disease, such as fever, chills, malaise and weight loss in about 43% of the patients. As the lesion progresses, skin becomes adhered to the mass and may rupture, forming a sinus and an open wound.
Diagnosis is usually performed by needle aspiration biopsy or excisional biopsy of the mass and the histological demonstration of stainable acid-fast bacteria in the case of infection by M. tuberculosis (Ziehl-Neelsen stain), or the culture of NTM using specific growth and staining techniques.
[External Links]
Information from eMedicine
Information from umm.edu
Information from MedlinePlus
Pulmonary Tuberculosis
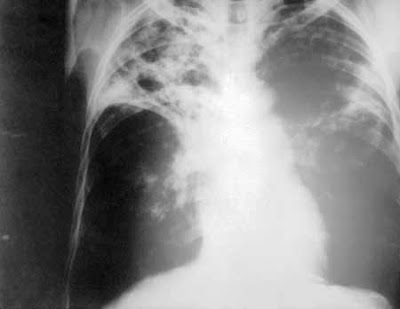 Pulmonary tuberculosis (TB) is a contagious bacterial infection that mainly involves the lungs, but may spread to other organs.
Pulmonary tuberculosis (TB) is a contagious bacterial infection that mainly involves the lungs, but may spread to other organs.Pulmonary tuberculosis is caused by the bacteria Mycobacterium tuberculosis (M. tuberculosis). You can get tuberculosis by breathing in air droplets from a cough or sneeze of an infected person.
Most people will recover from primary TB infection without further evidence of the disease. The infection may stay asleep or nonactive (dormant) for years and then reactivate.
Most people who develop symptoms of a TB infection first became infected in the past. However, in some cases, the disease may become active within weeks after the primary infection.
The following people are at higher risk for active TB: Elderly, Infants, People with weakened immune systems, for example due to AIDS, chemotherapy, or antirejection medicines given after an organ transplant.
The risk of contracting TB increases if you: Are in frequent contact with people who have the disease, Have poor nutrition, Live in crowded or unsanitary living conditions.
The following factors may increase the rate of TB infection in a population: Increase in HIV infections, Increase in number of homeless people (poor environment and nutrition), The appearance of drug-resistant strains of TB.
The primary stage of the disease usually doesn't have symptoms. When symptoms do occur, they may include: Cough (sometimes producing phlegm), Coughing up blood, Excessive sweating, especially at night, Fatigue, Fever, and Unintentional weight loss.
Other symptoms that may occur with this disease are breathing difficulty, chest pain, and wheezing.
[External Links]
Complete information from umm.edu
Information from healthguide.howstuffworks.com
More information from eMedicine
Tuberculosis
 Tuberculosis (abbreviated as TB for tubercle bacillus or Tuberculosis) is a common and often deadly infectious disease caused by mycobacteria, mainly Mycobacterium tuberculosis. Tuberculosis usually attacks the lungs (as pulmonary TB) but can also affect the central nervous system, the lymphatic system, the circulatory system, the genitourinary system, the gastrointestinal system, bones, joints, and even the skin. Other mycobacteria such as Mycobacterium bovis, Mycobacterium africanum, Mycobacterium canetti, and Mycobacterium microti also cause tuberculosis, but these species are less common.
Tuberculosis (abbreviated as TB for tubercle bacillus or Tuberculosis) is a common and often deadly infectious disease caused by mycobacteria, mainly Mycobacterium tuberculosis. Tuberculosis usually attacks the lungs (as pulmonary TB) but can also affect the central nervous system, the lymphatic system, the circulatory system, the genitourinary system, the gastrointestinal system, bones, joints, and even the skin. Other mycobacteria such as Mycobacterium bovis, Mycobacterium africanum, Mycobacterium canetti, and Mycobacterium microti also cause tuberculosis, but these species are less common.The classic symptoms of tuberculosis are a chronic cough with blood-tinged sputum, fever, night sweats, and weight loss. Infection of other organs causes a wide range of symptoms. The diagnosis relies on radiology (commonly chest X-rays), a tuberculin skin test, blood tests, as well as microscopic examination and microbiological culture of bodily fluids. Tuberculosis treatment is difficult and requires long courses of multiple antibiotics. Contacts are also screened and treated if necessary. Antibiotic resistance is a growing problem in (extensively) multi-drug-resistant tuberculosis. Prevention relies on screening programs and vaccination, usually with Bacillus Calmette-Guérin (BCG vaccine).
Tuberculosis is spread through the air, when people who have the disease cough, sneeze, or spit. One third of the world's current population has been infected with M. tuberculosis, and new infections occur at a rate of one per second. However, most of these cases will not develop the full-blown disease; asymptomatic, latent infection is most common. About one in ten of these latent infections will eventually progress to active disease, which, if left untreated, kills more than half of its victims.
[External Links]
Information from WHO
Information from bfhd.wa.gov
Information from familydoctor.org
Information from medicinenet.com
Hemorrhagic Fever
Any of a group of viral infections, including dengue hemorrhagic fever, Ebola virus disease, and yellow fever, that occur primarily in tropical climates, are usually transmitted to humans by arthropods or rodents, and are characterized by high fever, petechiae, internal bleeding, hypotension, and shock.
Viral hemorrhagic fevers are a group of illnesses that are caused by several distinct families of viruses: arenaviruses, filoviruses, bunyaviruses and flaviviruses. Some of these cause relatively mild illnesses, whilst others can cause severe, life-threatening disease.
Also known as H-Fever, Viral Hemorrhagic Fever, or VHF.
[External Links]
Information from hpa.org.uk
Information from Medline Plus
Viral hemorrhagic fevers are a group of illnesses that are caused by several distinct families of viruses: arenaviruses, filoviruses, bunyaviruses and flaviviruses. Some of these cause relatively mild illnesses, whilst others can cause severe, life-threatening disease.
Also known as H-Fever, Viral Hemorrhagic Fever, or VHF.
[External Links]
Information from hpa.org.uk
Information from Medline Plus
Typhoid Fever
 Typhoid fever, also known as enteric fever, or commonly just typhoid, is an illness caused by the bacterium Salmonella enterica serovar Typhi. Common worldwide, it is transmitted by the ingestion of food or water contaminated with feces from an infected person. The bacteria then perforate through the intestinal wall and are engulfed by macrophages. Salmonella Typhi then alters its structure to resist destruction and allow them to exist within the macrophage. This renders them resistant to damage by PMN's (Polymorphonuclear Leukocytes), complement and the immune response. The organism is then spread via the lymphatics while inside the macrophages. This gives them access to the reticuloendothelial system and then to the different organs throughout the body. The organism is a Gram-negative short bacillus that is motile due to its peritrichous flagella. The bacteria grows best at 37 °C/99 °F – human body temperature.
Typhoid fever, also known as enteric fever, or commonly just typhoid, is an illness caused by the bacterium Salmonella enterica serovar Typhi. Common worldwide, it is transmitted by the ingestion of food or water contaminated with feces from an infected person. The bacteria then perforate through the intestinal wall and are engulfed by macrophages. Salmonella Typhi then alters its structure to resist destruction and allow them to exist within the macrophage. This renders them resistant to damage by PMN's (Polymorphonuclear Leukocytes), complement and the immune response. The organism is then spread via the lymphatics while inside the macrophages. This gives them access to the reticuloendothelial system and then to the different organs throughout the body. The organism is a Gram-negative short bacillus that is motile due to its peritrichous flagella. The bacteria grows best at 37 °C/99 °F – human body temperature.Typhoid fever is characterized by a sustained fever as high as 40 °C (104 °F), profuse sweating, gastroenteritis, and non-bloody diarrhea. Less commonly a rash of flat, rose-colored spots may appear.
Classically, the course of untreated typhoid fever is divided into four individual stages, each lasting approximately one week. In the first week, there is a slowly rising temperature with relative bradycardia, malaise, headache and cough. A bloody nose (epistaxis) is seen in a quarter of cases and abdominal pain is also possible. There is leukopenia, a decrease in the number of circulating white blood cells, with eosinopenia and relative lymphocytosis, a positive diazo reaction and blood cultures are positive for Salmonella Typhi or Paratyphi. The classic Widal test is negative in the first week.
In the second week of the infection, the patient lies prostrated with high fever in plateau around 40 °C (104 °F) and bradycardia (Sphygmo-thermic dissociation), classically with a dicrotic pulse wave. Delirium is frequent, frequently calm, but sometimes agitated. This delirium gives to typhoid the nickname of "nervous fever". Rose spots appear on the lower chest and abdomen in around 1/3 patients. There are rhonchi in lung bases. The abdomen is distended and painful in the right lower quadrant where borborygmi can be heard. Diarrhea can occur in this stage: six to eight stools in a day, green with a characteristic smell, comparable to pea-soup. However, constipation is also frequent. The spleen and liver are enlarged (hepatosplenomegaly) and tender and there is elevation of liver transaminases. The Widal reaction is strongly positive with antiO and antiH antibodies. Blood cultures are sometimes still positive at this stage.
In the third week of typhoid fever a number of complications can occur: Intestinal hemorrhage due to bleeding in congested Peyer's patches; this can be very serious but is usually non-fatal. Intestinal perforation in distal ileum: this is a very serious complication and is frequently fatal. It may occur without alarming symptoms until septicemia or diffuse peritonitis sets in. Encephalitis, metastatic abscesses, cholecystitis, endocarditis and osteitis may also occur. The fever is still very high and oscillates very little over 24 hours. Dehydration ensues and the patient is delirious (typhoid state). By the end of third week the fever has started reducing (defervescence). This carries on into the fourth and final week.
[External Links]
Information from WHO
Information from MedlinePlus
Information from medicinenet.com
Information from eMedicine
Tangier Disease
 Tangier disease is a rare autosomal recessive condition characterized by low levels of high density lipoprotein cholesterol (HDL-C) in the blood, accumulation of cholesterol in many organs of the body, and an increased risk of arteriosclerosis.
Tangier disease is a rare autosomal recessive condition characterized by low levels of high density lipoprotein cholesterol (HDL-C) in the blood, accumulation of cholesterol in many organs of the body, and an increased risk of arteriosclerosis.TD is caused by mutations in the ABCA1 (ATP-binding cassette) gene on chromosome 9q31. ABCA1 codes for a protein that helps rid cells of excess cholesterol. This cholesterol is then picked up by HDL particles in the blood and carried to the liver, which processes the cholesterol to be reused in cells throughout the body. Individuals with TD are unable to eliminate cholesterol from cells, leading to its buildup in the tonsils and other organs.
The symptoms of Tangier disease are quite variable but the most common symptoms of Tangier disease are enlarged, yellow-colored tonsils, an enlarged spleen, accumulation of cholesterol in the mucous membranes of the intestines, abnormalities in the nervous system (neuropathy), and an increased risk of arteriosclerosis. Less commonly seen symptoms are an enlarged liver, lymph nodes and thymus, and hemolytic anemia. Cholesterol accumulation has been seen in other organs such as the bone marrow, gall bladder, skin, kidneys, heart valves, ureters, testicles, and the cornea of the eye.
Tangier disease is also known as A-alphalipoprotein Neuropathy.
[External Links]
More information from healthline.com
Get genetic-related information from genecards.org
More information Genetics Home Reference website
Hong Kong Flu
 The Hong Kong Flu was a category 2 flu pandemic caused by Influenza A with a subtype of H3N2 that descended from H2N2 by antigenic shift, in which genes from multiple subtypes re-assorted to form a new virus. The Hong Kong Flu pandemic of 1968 and 1969 infected an estimated 500,000 people with a low death rate. Fifty million people were infected in the United States, resulting in an estimated 34,000 deaths.
The Hong Kong Flu was a category 2 flu pandemic caused by Influenza A with a subtype of H3N2 that descended from H2N2 by antigenic shift, in which genes from multiple subtypes re-assorted to form a new virus. The Hong Kong Flu pandemic of 1968 and 1969 infected an estimated 500,000 people with a low death rate. Fifty million people were infected in the United States, resulting in an estimated 34,000 deaths.Both the H2N2 and H3N2 pandemic flu strains contained genes from avian influenza viruses. The new subtypes arose in pigs co-infected with avian and human viruses and were soon transferred to humans. Swine were considered the original "intermediate host" for influenza, because they supported re-assortment of divergent subtypes. However, other hosts appear capable of similar co-infection (e.g., many poultry species), and direct transmission of avian viruses to humans is possible.
The Hong Kong flu strain shared internal genes and the neuraminidase with the 1957 Asian Flu (H2N2). Accumulated antibodies to the neuraminidase or internal proteins may have resulted in much fewer casualties than most pandemics.
Symptoms of this flu is similar to common influenza, including Headache, Fever, Chills, Sneezing, Runny nose, Nasal inflammation, Blocked nose, Dry cough, Sore throat, Body aches, Muscle aches, Limb pain, Joint pain, Loss of appetite, and Myalgia. However, it may progress and lead to serious complications.
[External Links]
Information from medterms.com
Onchocerciasis
 Onchocerciasis also known as river blindness, is one the world's leading infectious cause of blindness. It is caused by Onchocerca volvulus, a nematode that can live for up to fifteen years in the human body. It is transmitted to people through the bite of a black fly. The worms spread throughout the body, and when they die, they cause intense itching and a strong immune system response that can destroy nearby tissue, such as the eye.
Onchocerciasis also known as river blindness, is one the world's leading infectious cause of blindness. It is caused by Onchocerca volvulus, a nematode that can live for up to fifteen years in the human body. It is transmitted to people through the bite of a black fly. The worms spread throughout the body, and when they die, they cause intense itching and a strong immune system response that can destroy nearby tissue, such as the eye.The primary treatment is a drug, ivermectin. For best effect, entire communities are treated at the same time. A single dose may kill first-stage larvae (microfilariae) in infected people and prevent transmission for many months in the remaining population.
[External Links]
Information from WHO
Information from emedicine.medscape.com
Information from merck.com
Calabar Swelling
 Calabar swellings are localized infections where the parasite Loa Loa is secreting toxins. It is an immune reaction caused when the worms that reside in the subcutaneous tissue are injured by a minor or major force to the skin. The insides of the worm are then exposed to the immune system, and a powerful reaction ensues. Normally, the immune system does not detect the helminth until it is injured.
Calabar swellings are localized infections where the parasite Loa Loa is secreting toxins. It is an immune reaction caused when the worms that reside in the subcutaneous tissue are injured by a minor or major force to the skin. The insides of the worm are then exposed to the immune system, and a powerful reaction ensues. Normally, the immune system does not detect the helminth until it is injured.See also Loa Loa Filariasis.
[External Links]
Information from fasthealth.com
Information from mondofacto.com
Loa Loa Filariasis
 Loa loa filariasis (also loiasis, loaiasis, Calabar swellings and African eyeworm) is a skin and eye disease caused by the nematode worm, loa loa filaria. Humans contract this disease through the bite of a Deer fly or Mango fly vector for Loa loa. The adult Loa loa filarial worm migrates throughout the subcutaneous tissues of humans, occasionally crossing into subconjunctival tissues where it can be easily observed. This presentation led to the popular name, African eye worm. Loa loa does not normally affect one’s vision but can be painful when moving about the eyeball or across the bridge of the nose. The disease can cause red itchy swellings below the skin called "Calabar swellings". The disease is treated with the drug diethylcarbamazine (DEC), and when appropriate, surgical methods may be employed to remove adult worms from the conjunctiva.
Loa loa filariasis (also loiasis, loaiasis, Calabar swellings and African eyeworm) is a skin and eye disease caused by the nematode worm, loa loa filaria. Humans contract this disease through the bite of a Deer fly or Mango fly vector for Loa loa. The adult Loa loa filarial worm migrates throughout the subcutaneous tissues of humans, occasionally crossing into subconjunctival tissues where it can be easily observed. This presentation led to the popular name, African eye worm. Loa loa does not normally affect one’s vision but can be painful when moving about the eyeball or across the bridge of the nose. The disease can cause red itchy swellings below the skin called "Calabar swellings". The disease is treated with the drug diethylcarbamazine (DEC), and when appropriate, surgical methods may be employed to remove adult worms from the conjunctiva.The treatment of choice for loiasis, diethylcarbamazine, can lead to serious complications in and of itself when administered in standard doses to patients with high Loa loa microfilarial loads.
Synonyms for the disease include African eye worm, Loaiasis, Loaina, Filaria loa, Filaria lacrimalis, Filaria subconjunctivalis, Calabar swellings, and Fugitive swellings. Loa loa, the scientific name for the infectious agent, is a "Native" term itself and it is likely that there are many other terms used from region to region.
[External Links]
Information from wrongdiagnosis.com
Broad information regarding the disease
Lymphatic Filariasis
 Lymphatic filariasis is a debilitating disease caused by nematode worms of the genera Wucheria and Brugia. Larval worms circulate in the bloodstream of infected persons, and adult worms live in the lymphatic vessels. Lymphatic filariasis is not life threatening, but it does cause discomfort, swelling of the limbs and genitals, damage to the kidneys and lymphatic system, impairment of the body's ability to fight infection, and general malaise. In addition, it causes immeasurable emotional and economic costs in terms of the disruption of family and community life.
Lymphatic filariasis is a debilitating disease caused by nematode worms of the genera Wucheria and Brugia. Larval worms circulate in the bloodstream of infected persons, and adult worms live in the lymphatic vessels. Lymphatic filariasis is not life threatening, but it does cause discomfort, swelling of the limbs and genitals, damage to the kidneys and lymphatic system, impairment of the body's ability to fight infection, and general malaise. In addition, it causes immeasurable emotional and economic costs in terms of the disruption of family and community life.Humans contract filariasis when they are bitten repeatedly by mosquitoes infected with filarial worms. Over 70 species of mosquitoes in the genera Culex, Anopheles, Aedes, and Mansoniacan infect humans with the disease. Mosquitoes pick up the tiny, microfilarial form of the parasite when taking blood meals from infected humans. In the mosquito, the microfilariae develop within 7-21 days into members of the next stage of the parasite's life cycle, which are known as filariform larva. The filariform larva are infective to humans. When the larval worms move to a mosquito's mouth, and then the mosquito bites humans, the parasites can spread through a human community. Fortunately, however, many bites from infected mosquitoes are required before a person is infected with the disease.
Once a human does pick up filariform larvae from mosquito bites, the larvae move to the lymphatic system, where they develop into adult worms. It usually takes 8-16 months after infection for symptoms of the disease to appear. The life span of adult worms is approximately seven years (microfilariae have a life span of from 3-36 months). The adults range in size from 2-50 cm in length. In the human, the adult worms mate and then the females produce millions of new microfilariae, which then circulate in the blood stream. Microfilariae circulating in the bloodstream can then be picked up by mosquitoes taking blood meals. In most endemic regions, microfilariae show peak abundance in the human bloodstream between 10 p.m. and 2 a.m., which corresponds with the time when Culex mosquitoes are most active. In some regions of the South Pacific, however, where the vectors of filariasis are active primarily in the daytime, microfilariae are most abundant during the day. These observations are consistent with the hypothesis that the microfilariae-abundance cycle in the bloodstream has evolved to maximize transmission to mosquitoes.
[External Links]
More Information from Boston College's website
More information from dhpe.org
More information from wrongdiagnosis.com
Filariasis
Filariasis is a parasitic and infectious tropical disease, that is caused by thread-like filarial nematode worms. These are divided into 3 groups according to the niche within the body that they occupy: Lymphatic Filariasis, Subcutaneous Filariasis, and Serous Cavity Filariasis. Lymphatic Filariasis is caused by the worms Wuchereria bancrofti, Brugia malayi, and Brugia timori. These worms occupy the lymphatic system, including the lymph nodes, and in chronic cases these worms lead to the disease Elephantiasis. Subcutaneous Filariasis is caused by Loa loa (the African eye worm), Mansonella streptocerca, Onchocerca volvulus, and Dracunculus medinensis (the guinea worm). These worms occupy the subcutaneous layer of the skin, the fat layer. Serous Cavity Filariasis is caused by the worms Mansonella perstans and Mansonella ozzardi, which occupy the serous cavity of the abdomen. In all cases, the transmitting vectors are either blood sucking insects (fly or mosquito) or Copepod crustaceans in the case of Dracunculus medinensis.
Human filarial nematode worms have a complicated life cycle, which primarily consists of five stages. After the male and female worm mate, the female gives birth to live microfilariae by the thousands. The microfilariae are taken up by the vector insect (intermediate host) during a blood meal. In the intermediate host, the microfilariae molt and develop into 3rd stage (infective) larvae. Upon taking another blood meal the vector insect injects the infectious larvae into the dermis layer of our skin. After approximately one year the larvae molt through 2 more stages, maturing into to the adult worm.
Individuals infected by filarial worms may be described as either "microfilaraemic" or "amicrofilaraemic," depending on whether or not microfilaria are found in their peripheral blood. Filariasis is diagnosed in microfilaraemic cases primarily through direct observation of microfilaria in the peripheral blood. Occult filariasis is diagnosed in amicrofilaraemic cases based on clinical observations and, in some cases, by finding a circulating antigen in the blood.
[External Links]
More information from emedicine.medscape.com
Human filarial nematode worms have a complicated life cycle, which primarily consists of five stages. After the male and female worm mate, the female gives birth to live microfilariae by the thousands. The microfilariae are taken up by the vector insect (intermediate host) during a blood meal. In the intermediate host, the microfilariae molt and develop into 3rd stage (infective) larvae. Upon taking another blood meal the vector insect injects the infectious larvae into the dermis layer of our skin. After approximately one year the larvae molt through 2 more stages, maturing into to the adult worm.
Individuals infected by filarial worms may be described as either "microfilaraemic" or "amicrofilaraemic," depending on whether or not microfilaria are found in their peripheral blood. Filariasis is diagnosed in microfilaraemic cases primarily through direct observation of microfilaria in the peripheral blood. Occult filariasis is diagnosed in amicrofilaraemic cases based on clinical observations and, in some cases, by finding a circulating antigen in the blood.
[External Links]
More information from emedicine.medscape.com
Aarskog-Scott Syndrome
 Aarskog-Scott syndrome is an inherited disease characterized by short stature, facial abnormalities, skeletal and genital anomalies.
Aarskog-Scott syndrome is an inherited disease characterized by short stature, facial abnormalities, skeletal and genital anomalies.The syndrome is named for Dagfinn Aarskog, a Norwegian pediatrician and human geneticist who first described it in 1970, and for Charles I. Scott, Jr., an American medical geneticist who independently described the syndrome in 1971.
Aarskog-Scott syndrome is transmitted in an X-linked recessive manner. The sons of female carriers are at 50% risk of being affected with the syndrome. The daughters of female carriers are at 50% risk of being carriers themselves. Females may have mild manifestations of the syndrome.
The Aarskog-Scott syndrome is a disorder with short stature, hypertelorism, downslanting palpebral fissures, anteverted nostrils, joint laxity, shawl scrotum, and mental retardation. The physical phenotype varies with age and postpuberal males may have only minor remnant manifestations of the prepuberal phenotype.
The Aarskog-Scott syndrome is also known as the Aarskog syndrome, Facial-digital-genital syndrome, faciodigitogenital syndrome, shawl scrotum syndrome and faciogenital dysplasia.
[External Links]
Get more information from MedlinePlus
More Information from University of Maryland Medical Center website
Information from wrongdiagnosis.com
Rhinorrhea
 Rhinorrhea, commonly known as a runny nose, consists of an unusually significant amount of nasal discharge. It is a symptom of the common cold and of allergies (hay fever).
Rhinorrhea, commonly known as a runny nose, consists of an unusually significant amount of nasal discharge. It is a symptom of the common cold and of allergies (hay fever).The term comes from the Greek words "rhinos" meaning "of the nose" and "rhoia" meaning "a flowing." Rhinorrhea can also be a sign of withdrawal, such as from opioids (especially methadone).
Rhinorrhea may be due to allergic conditions such as hay fever or foreign materials within the nostril. Bacterial or viral infections such as the common cold, influenza or sinusitis may also be accompanied by a runny nose. Nasal discharges may also be present in cases of vasomotor rhinitis, a non-infectious and non-allergenic condition.
Head injuries may also cause excess nasal discharges. Basilar skull fracture may result in cerebrospinal fluid rhinorrhea.
Environmental causes include contact with strong smelling substances such as disulfide compounds found in onions and garlic, both of the genus Allium. CS gas, which provides an especially intense pepper-like odor, also results in this symptom. This phenomenon is caused by the same mechanism that causes a runny nose when crying: tears drain through the inner corner of the eyelids through the nasolacrimal duct, and finally into the nasal cavity, where they manifest as a runny nose.
[External Links]
More information from bio-medicine.org
Information from mayoclinic.com
Information from medicinenet.com
Dengue Hemorrhagic Fever
 Dengue fever and dengue hemorrhagic fever (DHF) are acute febrile diseases, found in the tropics and Africa, and caused by four closely related virus serotypes of the genus Flavivirus, family Flaviviridae. It is also known as breakbone fever. Each serotype is sufficiently different that there is no cross-protection and epidemics caused by multiple serotypes (hyperendemicity) can occur. Dengue is transmitted to humans by the Aedes aegypti or more rarely the Aedes albopictus mosquito, which feed during the day.
Dengue fever and dengue hemorrhagic fever (DHF) are acute febrile diseases, found in the tropics and Africa, and caused by four closely related virus serotypes of the genus Flavivirus, family Flaviviridae. It is also known as breakbone fever. Each serotype is sufficiently different that there is no cross-protection and epidemics caused by multiple serotypes (hyperendemicity) can occur. Dengue is transmitted to humans by the Aedes aegypti or more rarely the Aedes albopictus mosquito, which feed during the day.The disease manifests as a sudden onset of severe headache, muscle and joint pains (myalgias and arthralgias—severe pain that gives it the nick-name break-bone fever or bonecrusher disease), fever, and rash. The dengue rash is characteristically bright red petechiae and usually appears first on the lower limbs and the chest; in some patients, it spreads to cover most of the body. There may also be gastritis with some combination of associated abdominal pain, nausea, vomiting, or diarrhea.
Some cases develop much milder symptoms which can be misdiagnosed as influenza or other viral infection when no rash is present. Thus travelers from tropical areas may pass on dengue in their home countries inadvertently, having not been properly diagnosed at the height of their illness. Patients with dengue can pass on the infection only through mosquitoes or blood products and only while they are still febrile.
The classic dengue fever lasts about six to seven days, with a smaller peak of fever at the trailing end of the disease (the so-called biphasic pattern). Clinically, the platelet count will drop until the patient's temperature is normal.
Cases of DHF also show higher fever, variable hemorrhagic phenomena, thrombocytopenia, and hemoconcentration. A small proportion of cases lead to dengue shock syndrome (DSS) which has a high mortality rate.
[External Links]
Information for Health Care Practitioners from cdc.gov
More Information from emedicine.medscape.com
Information from doh.gov.ph
Zadik Barak Levin Syndrome
Zadik Barak Levin Syndrome (ZBLS) is a congenital disorder in humans. It is the result of an embryonic defect in the mesodermal-ectodermal midline development.
Signs include dermoid cysts, abdominal swelling, abdominal fullness, abdominal pain, hypothyroidism, weakness, cold intolerance, decreased memory, constipation, muscle cramps, hearing impairment, depression, hoarseness, macroglossia, absence of teeth, facial deformity, facial abnormality, cleft palate, menstrual abnormalities.
[External Links]
More information from wrongdiagnosis.com
Information from ailments.com
Signs include dermoid cysts, abdominal swelling, abdominal fullness, abdominal pain, hypothyroidism, weakness, cold intolerance, decreased memory, constipation, muscle cramps, hearing impairment, depression, hoarseness, macroglossia, absence of teeth, facial deformity, facial abnormality, cleft palate, menstrual abnormalities.
[External Links]
More information from wrongdiagnosis.com
Information from ailments.com
SHORT Syndrome
SHORT syndrome is a medical condition in which affected individuals have multiple birth defects in different organ systems.
SHORT is an acronym for short stature, hyperextensibility of joints and/or inguinal hernia, ocular depression, Rieger anomaly and teething delay.
Other characteristics common in SHORT syndrome are a triangular face, small chin with a dimple, a loss of fat under the skin (lipodystrophy), abnormal position of the ears, hearing loss and delayed speech.
[External Links]
More information from wrongdiagnosis.com
SHORT is an acronym for short stature, hyperextensibility of joints and/or inguinal hernia, ocular depression, Rieger anomaly and teething delay.
Other characteristics common in SHORT syndrome are a triangular face, small chin with a dimple, a loss of fat under the skin (lipodystrophy), abnormal position of the ears, hearing loss and delayed speech.
[External Links]
More information from wrongdiagnosis.com
Aarskog-Ose-Pande Syndrome
Aarskog-Ose-Pande syndrome is a rare disorder involving lipodystrophy mainly in the face and buttocks as well as sparse hair, retarded bone age and minor face and eye anomalies. It is considered a variant of SHORT syndrome which tends to also include increased range of joint motion and more extensive lipodystrophy.
[External Links]
Get more information from wrongdiagnosis.com
Information from Google Health
[External Links]
Get more information from wrongdiagnosis.com
Information from Google Health
Malaria
 Malaria is a vector-borne infectious disease that is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa.
Malaria is a vector-borne infectious disease that is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa.Malaria is one of the most common infectious diseases and an enormous public health problem. The disease is caused by protozoan parasites of the genus Plasmodium. Four types of the plasmodium parasite can infect humans; the most serious forms of the disease are caused by Plasmodium falciparum and Plasmodium vivax, but other related species (Plasmodium ovale, Plasmodium malariae) can also affect humans. This group of human-pathogenic Plasmodium species is usually referred to as malaria parasites.
Usually, people get malaria by being bitten by an infective female Anopheles mosquito. Only Anopheles mosquitoes can transmit malaria, and they must have been infected through a previous blood meal taken on an infected person. When a mosquito bites an infected person, a small amount of blood is taken, which contains microscopic malaria parasites. About one week later, when the mosquito takes its next blood meal, these parasites mix with the mosquito's saliva and are injected into the person being bitten. The parasites multiply within red blood cells, causing symptoms that include symptoms of anemia (light-headedness, shortness of breath, tachycardia, etc.), as well as other general symptoms such as fever, chills, nausea, flu-like illness, and, in severe cases, coma, and death. Malaria transmission can be reduced by preventing mosquito bites with mosquito nets and insect repellents, or by mosquito control measures such as spraying insecticides inside houses and draining standing water where mosquitoes lay their eggs.
Malaria infections are treated through the use of antimalarial drugs, such as quinine or artemisinin derivatives. However, parasites have evolved to be resistant to many of these drugs.
[External Links]
Information regarding Malaria from WHO
Complete Information from MedlinePlus
Complete Information from eMedicine
Fever
Fever refers to an elevation in normal body temperature. Technically, any body temperature above the normal oral measurement of 98.6 °F (37 °C) or the normal rectal temperature of 99 °F (37.2 °C) is considered to be elevated. However, these are averages, and your normal temperature may actually be 1 °F (0.6 °C) or more above or below the average of 98.6 °F. Body temperature can also vary up to 1 °F (0.6 °C) throughout the day.
Thus, fever is not considered medically significant until body temperature is above 100.4 °F (38 °C). Fever serves as one of the body's natural defenses against bacteria and viruses which cannot live at a higher temperature. For that reason, low fevers should normally go untreated, unless accompanied by troubling symptoms.
Also, the body's defense mechanisms seem to work more efficiently at a higher temperature. Fever is just one part of an illness, many times no more important than the presence of other symptoms such as cough, sore throat, etc.
Fevers of 104 °F (40 °C) or higher demand immediate home treatment and subsequent medical attention, as they can result in delirium and convulsions, particularly in children.
[External Links]
Read more about fever here
Read about fever from MedlinePlus
Flowchart of things to do when having fever
Thus, fever is not considered medically significant until body temperature is above 100.4 °F (38 °C). Fever serves as one of the body's natural defenses against bacteria and viruses which cannot live at a higher temperature. For that reason, low fevers should normally go untreated, unless accompanied by troubling symptoms.
Also, the body's defense mechanisms seem to work more efficiently at a higher temperature. Fever is just one part of an illness, many times no more important than the presence of other symptoms such as cough, sore throat, etc.
Fevers of 104 °F (40 °C) or higher demand immediate home treatment and subsequent medical attention, as they can result in delirium and convulsions, particularly in children.
[External Links]
Read more about fever here
Read about fever from MedlinePlus
Flowchart of things to do when having fever
Influenza
 Influenza, commonly known as the flu, is an infectious disease that affects birds and mammals, caused by RNA viruses of the family Orthomyxoviridae (the influenza viruses). The name influenza comes from the Italian: influenza, meaning "influence", (Latin: influentia). In humans, common symptoms of the disease are chills, fever, pharyngitis, muscle pains, severe headache, coughing, weakness, and general discomfort. In more serious cases, influenza causes pneumonia, which can be fatal, particularly in young children and the elderly. Although it is often confused with the common cold, influenza is a much more severe disease and is caused by a different type of virus. Influenza can produce nausea and vomiting, especially in children, but these symptoms are more characteristic of the unrelated gastroenteritis, which is sometimes called "stomach flu" or "24-hour flu".
Influenza, commonly known as the flu, is an infectious disease that affects birds and mammals, caused by RNA viruses of the family Orthomyxoviridae (the influenza viruses). The name influenza comes from the Italian: influenza, meaning "influence", (Latin: influentia). In humans, common symptoms of the disease are chills, fever, pharyngitis, muscle pains, severe headache, coughing, weakness, and general discomfort. In more serious cases, influenza causes pneumonia, which can be fatal, particularly in young children and the elderly. Although it is often confused with the common cold, influenza is a much more severe disease and is caused by a different type of virus. Influenza can produce nausea and vomiting, especially in children, but these symptoms are more characteristic of the unrelated gastroenteritis, which is sometimes called "stomach flu" or "24-hour flu".Typically, influenza is transmitted from infected mammals through the air by coughs or sneezes, creating aerosols containing the virus, and from infected birds through their droppings. Influenza can also be transmitted by saliva, nasal secretions, feces and blood. Infections also occur through contact with these body fluids or with contaminated surfaces. Flu viruses can remain infectious for about one week at human body temperature, over 30 days at 0 °C (32 °F), and for much longer periods at very low temperatures. Most influenza strains can be inactivated easily by disinfectants and detergents.
The virus that causes influenza has the ability to mutate, creating new strains that are sometimes more potent than their predecessors. Example of the lethal strains is the H5N1, also known as the avian flu or bird flu.
Influenza occurs mostly in winter and during the tropical rainy season.
[External Links]
Information about flu from MedlinePlus
Information from WHO website
Information from Victorian Government Health Information website
Cough
 A Cough (Latin: tussis), is a sudden and often repetitively occurring defense reflex which helps to clear the large breathing passages from excess secretions, irritants, foreign particles and microbes. The cough reflex consists of three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound. Coughing can happen voluntarily as well as involuntarily, though for the most part, involuntarily.
A Cough (Latin: tussis), is a sudden and often repetitively occurring defense reflex which helps to clear the large breathing passages from excess secretions, irritants, foreign particles and microbes. The cough reflex consists of three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound. Coughing can happen voluntarily as well as involuntarily, though for the most part, involuntarily.Frequent or severe coughing usually indicates the presence of a disease. Many viruses and bacteria benefit by causing their host to cough, which helps to spread the disease to new hosts. Coughing is classified as acute (of sudden onset) if it is present less than three weeks, subacute if it is present between three and eight weeks, and chronic when lasting longer than eight weeks. A cough can be dry or productive, depending on whether sputum is coughed up. Most of the time, coughing is acute and caused by a respiratory tract infection. Coughing can be triggered by food entering the windpipe rather than the esophagus due to a failure of the epiglottis in patients who have difficulties swallowing. Smoking and air pollution are common causes of coughing. Provided the patient is a non-smoker and has a normal chest X-ray, the three most common causes of chronic cough are asthma, gastroesophageal reflux disease and post-nasal drip. Other causes of chronic cough include chronic bronchitis, heart failure and medications such as ACE inhibitors.
Since cough is a natural protective reflex, suppressing the cough reflex might have deleterious effects, especially if the cough is productive. Nonetheless, coughing might be severe enough (in terms of psychological, physical and social distress) to warrant treatment. This should be targeted towards the cause as much as possible, for example by smoking cessation and discontinuing ACE inhibitors. Some patients may only be worried about serious illnesses, and reassurance may suffice. Cough suppressants (or antitussives) such as codeine or dextromethorphan are frequently prescribed although scientific evidence supporting their use is often of poor quality. Other treatment options may target airway inflammation or may promote mucus expectoration.
[External Links]
Broader information regarding cough
Information from MedlinePlus
Flowchart of things you have to do when you have cough
Lymphedema
 Lymphedema, also known as lymphatic obstruction, is a notoriously debilitating progressive condition. The unfortunate patient faces a lifelong struggle of medical, and sometimes surgical, treatment fraught with potentially lethal complications.
Lymphedema, also known as lymphatic obstruction, is a notoriously debilitating progressive condition. The unfortunate patient faces a lifelong struggle of medical, and sometimes surgical, treatment fraught with potentially lethal complications.The underlying problem is lymphatic dysfunction, resulting in an abnormal accumulation of interstitial fluid containing high molecular weight proteins. This condition underscores the tremendous importance of a normally functioning lymphatic system, which returns proteins, lipids, and accompanying water from the interstitium to the venous circulation near the subclavian vein - internal jugular vein junction, bilaterally. The danger with lymphedema comes from the constant risk of developing an uncontrolled infection in the affected limb.
Symptoms of this disease may include fatigue, a heavy swollen limb or localized fluid acumulation in other body areas, including the head or neck, discoloration of the skin overlying the lymphedema, and eventually deformity (elephantiasis).
[External Links]
Information from emedicine.medscape.com
Information from mayoclinic.com
Peptic Ulcer
A Peptic Ulcer, also known as ulcus pepticum, PUD or peptic ulcer disease, is an ulcer (defined as mucosal erosion equal to or greater than 0.5 cm) of an area of the gastrointestinal tract that is usually acidic and thus extremely painful. As much as 80% of ulcers are associated with Helicobacter pylori, a spiral-shaped bacterium that lives in the acidic environment of the stomach, however only 20% of those cases go to a doctor. Ulcers can be also caused or worsened by drugs such as aspirin and other NSAIDs. Contrary to general belief, more peptic ulcers arise in the duodenum (first part of the small intestine, just after the stomach) than in the stomach. About 4% of stomach ulcers are caused by a malignant tumor, so multiple biopsies are needed to make sure. Duodenal ulcers are generally benign.
A peptic ulcer may be classified base on the location where it may arise. In Stomach (Gastric ulcer), Duodenum (Duodenal ulcer), Esophagus (Esophageal ulcer), and Meckel's Diverticulum (Meckel's Diverticulum ulcer).
[External Links]
Information derived from acg.gi.org
Information taken from Medline Plus
Information derived from foundationsurgery.com
A peptic ulcer may be classified base on the location where it may arise. In Stomach (Gastric ulcer), Duodenum (Duodenal ulcer), Esophagus (Esophageal ulcer), and Meckel's Diverticulum (Meckel's Diverticulum ulcer).
[External Links]
Information derived from acg.gi.org
Information taken from Medline Plus
Information derived from foundationsurgery.com
Gastric Ulcer
 A Gastric Ulcer, also called a stomach ulcer, is a raw, eroded area in the lining of the stomach.
A Gastric Ulcer, also called a stomach ulcer, is a raw, eroded area in the lining of the stomach.A gastric ulcer develops when stomach acids and digestive juices injure the stomach's lining of protective mucus. Gastric ulcers, most commonly, are caused by the use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen. Aspirin is the NSAID most likely to cause ulcers.
Gastric ulcers may also develop from the presence of bacteria called Helicobacter pylori (H. pylori), decreased resistance of the lining of the stomach to gastric acids, increased production of gastric acids and infection, certain types of medication, and disorders that cause over secretion of stomach juices. Ulcer can also be caused by the use of tobacco, alcohol, and caffeine.
The symptoms of gastric ulcers include indigestion and heartburn in the middle of the upper abdomen, nausea and loss of appetite, weight loss and repeated episodes of gastrointestinal bleeding. About 30% of patients with gastric ulcers are awakened by pain at night. Many patients have periods of chronic ulcer pain alternating with symptom-free periods that last for several weeks or months. The pain may be relieved by eating or taking antacids, and may get worse a couple of hours after meals or before meals.
If the gastric ulcer is bleeding, the patient may vomit bright red blood or digested blood that looks like brown coffee grounds and have black, tarry bowel movements.
[External Links]
Information on gastric ulcer from an educational site
Information on gastric ulcer from Medline Plus
Information on gastric ulcer from foundationsurgery.com
Information complete with Radiographic images from emedicine.medscape.com
Endoscopy of two giant gastric ulcers from youtube.com
Duodenal Ulcer
 Duodenal Ulcer is a common condition characterized by the presence of a well-demarcated break in the mucosa that may extend into the muscularis propria of the duodenum. More than 95% of duodenal ulcers are found in the first part of the duodenum; most are less than 1 cm in diameter.
Duodenal Ulcer is a common condition characterized by the presence of a well-demarcated break in the mucosa that may extend into the muscularis propria of the duodenum. More than 95% of duodenal ulcers are found in the first part of the duodenum; most are less than 1 cm in diameter.A duodenal ulcer is caused by stomach acid and digestive juices. A type of bacteria called Helicobacter pylori, also called H. pylori, commonly causes this. Other common causes of duodenal ulcers include anti-inflammatory medications such as aspirin and ibuprofen, stress, nicotine, caffeine, and alcohol use.
The symptoms of duodenal ulcers include heartburn, stomach pain relieved by eating or taking antacids, weight gain, and a burning sensation of the back of the throat. The patient is most likely to feel discomfort two to four hours after meals, or after having citrus juice, coffee, or aspirin. About fifty percent of patients with duodenal ulcers awake during the night with pain, usually between midnight and three a.m.
If an ulcer is bleeding, the patient may have vomit containing bright red blood or digested blood that looks like brown coffee ground and black, tarry bowel movements.
Proper diagnosis of duodenal ulcer is important because prompt initiation of treatment can effectively prevent potentially serious complications.
[External Links]
Complete information regarding duodenal ulcer
Video of a duodenal ulcer from youtube.com
More images and information of duodenal ulcer
Ulceration
The process or fact of being eroded away, as by an ulcer.
In medicine, Ulceration may refer to:
· Ulcer (dermatology), a discontinuity of the skin (see also Decubitus Ulcer).
· Oral Ulcer, an open sore inside the mouth.
· Peptic Ulcer, a discontinuity of the gastrointestinal mucosa.
· Corneal Ulcer, an inflammatory or infective condition of the cornea.
· Venous Ulcer, a wound thought to occur due to improper functioning of valves in the veins.
· Genital Ulcer, an ulcer located on the genital area.
[External Links]
Information taken from medterms.com
In medicine, Ulceration may refer to:
· Ulcer (dermatology), a discontinuity of the skin (see also Decubitus Ulcer).
· Oral Ulcer, an open sore inside the mouth.
· Peptic Ulcer, a discontinuity of the gastrointestinal mucosa.
· Corneal Ulcer, an inflammatory or infective condition of the cornea.
· Venous Ulcer, a wound thought to occur due to improper functioning of valves in the veins.
· Genital Ulcer, an ulcer located on the genital area.
[External Links]
Information taken from medterms.com
Decubitus Ulcer
 A Decubitus Ulcer is a pressure sore or what is commonly called a "bedsore". It can range from a very mild pink coloration of the skin, which disappears in a few hours after pressure is relieved on the area, to a very deep wound extending to the subcutaneous layer, and sometimes through a bone or into internal organs. These ulcers, as well as other wound types, are classified in stages according to the severity of the wound.
A Decubitus Ulcer is a pressure sore or what is commonly called a "bedsore". It can range from a very mild pink coloration of the skin, which disappears in a few hours after pressure is relieved on the area, to a very deep wound extending to the subcutaneous layer, and sometimes through a bone or into internal organs. These ulcers, as well as other wound types, are classified in stages according to the severity of the wound.These lesions may be caused by many factors such as: unrelieved pressure; friction; humidity; shearing forces; temperature; age; continence and medication, to any part of the body, especially portions over bony or cartilaginous areas such as sacrum, elbows, knees, ankles, etc. Although easily prevented and completely treatable if found early, bedsores are often fatal - even under the auspices of medical care - and are one of the leading iatrogenic causes of death reported in developed countries, second only to adverse drug reactions.
[External Links]
Information derived from nlm.nih.gov
Prevention and Treatment of Bedsores
Complete information about Decubitus Ulcer from emedicine.medscape.com
Aagenaes Syndrome
An idiopathic form of familial intrahepatic cholestasis associated with lymphedema of the lower extremities.
It is a syndrome characterized by congenital hypoplasia of lymph vessels, which causes lymphedema of the legs and recurrent cholestasis in infancy, and slow progress to hepatic cirrhosis and giant-cell hepatitis with fibrosis of the portal tracts.
It is autosomal recessively inherited. A common feature of the condition is generalized lymphatic anomaly, which may be indicative of the defect being lymphangiogenetic in origin. It is named after Oystein Aagenaes, a Norwegian pediatrician. It is also called cholestasis-lymphedema syndrome (CLS).
[External Links]
Information from wrongdiagnosis.com
Support information from ncbi.nlm.nih.gov
It is a syndrome characterized by congenital hypoplasia of lymph vessels, which causes lymphedema of the legs and recurrent cholestasis in infancy, and slow progress to hepatic cirrhosis and giant-cell hepatitis with fibrosis of the portal tracts.
It is autosomal recessively inherited. A common feature of the condition is generalized lymphatic anomaly, which may be indicative of the defect being lymphangiogenetic in origin. It is named after Oystein Aagenaes, a Norwegian pediatrician. It is also called cholestasis-lymphedema syndrome (CLS).
[External Links]
Information from wrongdiagnosis.com
Support information from ncbi.nlm.nih.gov
ABCD Syndrome
ABCD Syndrome is a rare inherited condition characterized by albinism, deafness, a black lock of hair, and intestinal abnormalities.
ABCD is an acronym for albinism, black lock, cell migration disorder of the neurocytes of the gut and sensorineural deafness. It has been found to be caused by mutation in the endothelin B receptor gene (EDNRB).
[External Links]
Information from wrongdiagnosis.com
Genetic related Information of the disease from genecards.org
Disease Information from ncbi.nlm.nih.gov
ABCD is an acronym for albinism, black lock, cell migration disorder of the neurocytes of the gut and sensorineural deafness. It has been found to be caused by mutation in the endothelin B receptor gene (EDNRB).
[External Links]
Information from wrongdiagnosis.com
Genetic related Information of the disease from genecards.org
Disease Information from ncbi.nlm.nih.gov
Link to Us
Any site, as long as medical-related, may exchange links with us. We are, however, not open for now, as we are still in the process of building up.
Miscellaneous Links:
BlogLookup!
Miscellaneous Links:
BlogLookup!
About Disease Encyclopedia
Disease Encyclopedia is maintained by a group of nurses led by A.L. Yap, R.N. and supervised by Dr. D. Stinson. The Site was created to help researchers and medical practitioners by providing medical "disease" related information, and medical updates. As we all know, the Internet is a broad research ground, making it difficult for our researchers to obtain the information they need. However, through this blog site, we hope to make it easier for those seeking information to get what they want to find by collecting the information from the web and bring it in one place. We could also help widen your research by providing you referral links that may lead to a reliable source. For now, our site can only help with researches related to disease, we hope to bring more in the future.
Disclaimer
Disease Encyclopedia is a blog site opened to support researchers and medical practitioners by providing medical "disease" related information and resources. It does not, however, give medical advices. All materials (content) on the site are for informational purposes only.
As a blog, we allow comments to be made by the users, we are not, however, liable of what the commenters may have to say. We advice people to always seek professional help from certified physicians and not seek council from online users as such information may be erroneous and may result to demise.
The Site contents are base on facts and information derived from other sites or any other resource materials, and have been researched thoroughly to make sure its accuracy. We do not wish to disseminate false information that could ruin the purpose of this Site. We, however, advice our visitors to research their work thoroughly using other resource materials, as we may also be subject to human error. Please let us know if there are any erroneous information in the Site.
As a blog, we allow comments to be made by the users, we are not, however, liable of what the commenters may have to say. We advice people to always seek professional help from certified physicians and not seek council from online users as such information may be erroneous and may result to demise.
The Site contents are base on facts and information derived from other sites or any other resource materials, and have been researched thoroughly to make sure its accuracy. We do not wish to disseminate false information that could ruin the purpose of this Site. We, however, advice our visitors to research their work thoroughly using other resource materials, as we may also be subject to human error. Please let us know if there are any erroneous information in the Site.
News Archive
Our News Archive stores all recent and past medical news in chronological order. These have been verified and it all came from reliable sources.
Exposure to Air Pollution during pregnancy may curb Fetal Growth (April 12, 2009)
Locking Parasites in Host Cell could be new way to fight Malaria (April 4, 2009)
Progress toward an Alzheimer's Drug that saves Brain Cells (March 22, 2009)
Exposure to Air Pollution during pregnancy may curb Fetal Growth (April 12, 2009)
Locking Parasites in Host Cell could be new way to fight Malaria (April 4, 2009)
Progress toward an Alzheimer's Drug that saves Brain Cells (March 22, 2009)
List of Diseases
Welcome to Disease Encyclopedia, a Site created to bring you all medical "disease" related information. Throughout history, there had been numerous diseases discovered, some of it had been found a cure, while some of it remained incurable. Our database lists them in alphabetical order for an easy search.
1
11 Beta Hydroxylase Deficiency
1918 Flu Pandemic
A
Acid Reflux Disease
A-alphalipoprotein Neuropathy
Aarskog Syndrome
Aarskog-Ose-Pande Syndrome
Aarskog-Scott Syndrome
AAS
Aagenaes Syndrome
Aase Syndrome
Aase-Smith Syndrome
ABCD Syndrome
Abdominal Cramp
Abdominal Pain
Acute Gastroenteritis
African Eyeworm
Aneurysm
B
Bedsore
Bellyache
Break-Bone Fever
C
Calabar Swelling
Cholestasis-Lymphedema Syndrome
Colic
Consumption
Cough
D
Decubitus Ulcer
Dengue Fever
Dengue Hemorrhagic Fever
DHF
Duodenal Ulcer
E
Enteric Fever
Eye Worm
F
Facial-Digital-Genital Syndrome
Faciodigitogenital Syndrome
Faciogenital Dysplasia
Fever
Filaria Lacrimalis
Filaria Loa
Filariasis
Filaria Subconjunctivalis
Flu
Fugitive Swelling
G
Gastric Flu
Gastric Ulcer
Gastric Reflux Disease
Gastroenteritis
Gastroesophageal Reflux Disease
Gastro-oesophageal Reflux Disease
GERD
GORD
H
Hemorrhagic Fever
H-Fever
Hong Kong Flu
I
Influenza
Intestinal TB
Intestinal Tuberculosis
K
King's Evil
Koch's Disease
L
La Grippe
Loaiasis
Loa Loa Filariasis
Loiasis
Lymphatic Filariasis
Lymphatic Obstruction
Lymphedema
Lymphoedema
M
Malaria
O
Onchocerciasis
P
Peptic Ulcer
Peptic Ulcer Disease
Phthisis
Phthisis Pulmonalis
Pressure Ulcer
PUD
Pulmonary Tuberculosis
R
Rhinorrhea
River Blindness
Runny Nose
S
Scrofula
Shawl Scrotum Syndrome
SHORT Syndrome
Spanish Flu
Stomach Flu
Stomach Ulcer
T
Tangier Disease
TB
TD
Tuberculosis
Tummy Bug
Typhoid Fever
U
Ulcer
Ulceration
V
VHF
Viral Hemorrhagic Fever
Z
Zadik Barak Levin Syndrome
ZBLS
1
11 Beta Hydroxylase Deficiency
1918 Flu Pandemic
A
Acid Reflux Disease
A-alphalipoprotein Neuropathy
Aarskog Syndrome
Aarskog-Ose-Pande Syndrome
Aarskog-Scott Syndrome
AAS
Aagenaes Syndrome
Aase Syndrome
Aase-Smith Syndrome
ABCD Syndrome
Abdominal Cramp
Abdominal Pain
Acute Gastroenteritis
African Eyeworm
Aneurysm
B
Bedsore
Bellyache
Break-Bone Fever
C
Calabar Swelling
Cholestasis-Lymphedema Syndrome
Colic
Consumption
Cough
D
Decubitus Ulcer
Dengue Fever
Dengue Hemorrhagic Fever
DHF
Duodenal Ulcer
E
Enteric Fever
Eye Worm
F
Facial-Digital-Genital Syndrome
Faciodigitogenital Syndrome
Faciogenital Dysplasia
Fever
Filaria Lacrimalis
Filaria Loa
Filariasis
Filaria Subconjunctivalis
Flu
Fugitive Swelling
G
Gastric Flu
Gastric Ulcer
Gastric Reflux Disease
Gastroenteritis
Gastroesophageal Reflux Disease
Gastro-oesophageal Reflux Disease
GERD
GORD
H
Hemorrhagic Fever
H-Fever
Hong Kong Flu
I
Influenza
Intestinal TB
Intestinal Tuberculosis
K
King's Evil
Koch's Disease
L
La Grippe
Loaiasis
Loa Loa Filariasis
Loiasis
Lymphatic Filariasis
Lymphatic Obstruction
Lymphedema
Lymphoedema
M
Malaria
O
Onchocerciasis
P
Peptic Ulcer
Peptic Ulcer Disease
Phthisis
Phthisis Pulmonalis
Pressure Ulcer
PUD
Pulmonary Tuberculosis
R
Rhinorrhea
River Blindness
Runny Nose
S
Scrofula
Shawl Scrotum Syndrome
SHORT Syndrome
Spanish Flu
Stomach Flu
Stomach Ulcer
T
Tangier Disease
TB
TD
Tuberculosis
Tummy Bug
Typhoid Fever
U
Ulcer
Ulceration
V
VHF
Viral Hemorrhagic Fever
Z
Zadik Barak Levin Syndrome
ZBLS
Subscribe to:
Posts (Atom)